Blank Tb Test PDF Form
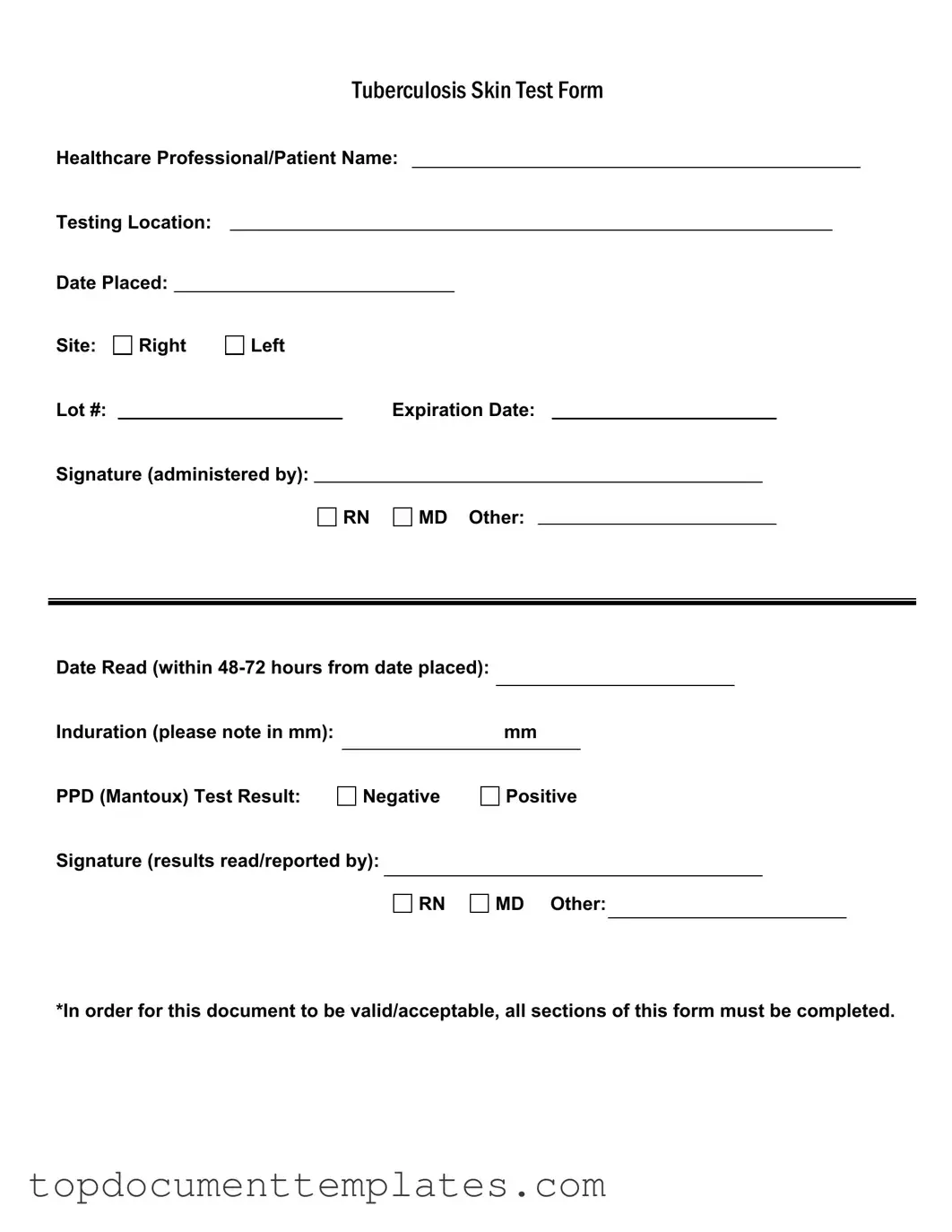
The Tuberculosis (TB) Test Form plays a crucial role in the assessment and management of TB exposure, particularly in healthcare settings and other environments where individuals may be at higher risk. This form captures essential information, including the names of both the healthcare professional and patient, as well as the testing location. It outlines key details such as the date the test was placed, the specific site on the body where the test was administered, and the lot number along with its expiration date, ensuring traceability and validity of the test materials used. Additionally, the form requires the signature of the administering professional, which can be an RN, MD, or other qualified personnel, thereby confirming that the test was conducted according to established protocols. After the test is placed, it is critical to read the results within 48 to 72 hours, a timeframe noted on the form, where the induration, measured in millimeters, is documented. The outcome of the PPD (Mantoux) test is clearly indicated as either negative or positive, providing vital information for further medical evaluation. Lastly, the form must be fully completed for it to be valid, reinforcing the importance of thorough documentation in healthcare practices.
Similar forms
Immunization Record: Similar to the TB Test form, an immunization record documents vaccinations received by a patient. It includes details such as the vaccine type, administration date, and healthcare provider's signature.
Medical History Form: This form collects comprehensive information about a patient's past medical conditions and treatments. Like the TB Test form, it requires completion of all sections to be valid.
Consent Form: A consent form ensures that patients agree to a specific medical procedure or treatment. It includes patient information and requires signatures, similar to the TB Test form.
Patient Registration Form: This document gathers essential information about a new patient, such as contact details and insurance information. It must be fully completed for proper processing, just like the TB Test form.
Referral Form: A referral form is used when a healthcare provider recommends a patient to a specialist. It includes patient details and requires signatures, paralleling the TB Test form's structure.
- Articles of Incorporation Form: This document is vital for establishing a corporation in New York, detailing the company's name, purpose, and structure. For further information, you can visit documentonline.org/blank-new-york-articles-of-incorporation/.
Lab Test Order Form: This form requests specific laboratory tests for a patient. It must be filled out completely, similar to the TB Test form, to ensure accurate processing of test results.
Discharge Summary: A discharge summary provides a summary of a patient's hospital stay, including treatments and follow-up care. It is a comprehensive document that requires all sections to be filled out, akin to the TB Test form.
Guidelines on Writing Tb Test
Completing the TB Test form is a straightforward process that requires accurate information. After filling out the form, it will be submitted for record-keeping and further medical evaluation if necessary. Follow the steps below to ensure all required sections are completed properly.
- Healthcare Professional/Patient Name: Write the full name of the healthcare professional administering the test or the patient's name, depending on who is being tested.
- Testing Location: Indicate the location where the test is being conducted.
- Date Placed: Enter the date when the test was administered.
- Site: Mark whether the test was placed on the right or left arm.
- Lot #: Fill in the lot number of the PPD solution used for the test.
- Expiration Date: Write the expiration date of the PPD solution.
- Signature (administered by): The healthcare professional administering the test should sign here. Indicate their title (RN, MD, or Other).
- Date Read: Note the date when the test results are read, which should be within 48-72 hours from the date placed.
- Induration: Measure the induration in millimeters and write the measurement in the space provided.
- PPD (Mantoux) Test Result: Circle or mark whether the result is negative or positive.
- Signature (results read/reported by): The healthcare professional who reads the results should sign here. Indicate their title (RN, MD, or Other).
Ensure that all sections are filled out completely for the document to be valid and acceptable. Double-check your entries before submission.
Form Data
| Fact Name | Description |
|---|---|
| Form Purpose | The Tuberculosis Skin Test Form is used to document the administration and results of the PPD (Mantoux) test. |
| Healthcare Professional Signature | The form must be signed by a qualified healthcare professional, such as a registered nurse (RN) or medical doctor (MD). |
| Testing Location | The specific location where the test is administered must be recorded on the form. |
| Date Placed | The date the PPD test is administered must be clearly indicated on the form. |
| Date Read | The results must be read and recorded within 48 to 72 hours after the test is placed. |
| Induration Measurement | The size of the induration, measured in millimeters, must be noted to determine the test result. |
| Test Result | The PPD test result is categorized as either negative or positive, which must be documented on the form. |
| Lot Number | The lot number of the PPD test must be recorded for tracking and quality control purposes. |
| Expiration Date | The expiration date of the PPD test must be noted to ensure the validity of the results. |
| Compliance Requirement | All sections of the Tuberculosis Skin Test Form must be completed for it to be valid and acceptable. |
Other PDF Documents
How to Make Pay Stubs If Self Employed - Contains a summary of earnings necessary for gathering business insights.
The Florida Employment Verification form is essential for employers to validate their employees' eligibility to work in the United States. This document not only helps in complying with federal and state employment laws but also safeguards the integrity of the labor market. For more information on the process and requirements, employers can refer to resources such as OnlineLawDocs.com.
Affidavit of Death of Joint Tenant - The affidavit helps ensure compliance with state laws regarding joint property.