Blank Medication Administration Record Sheet PDF Form
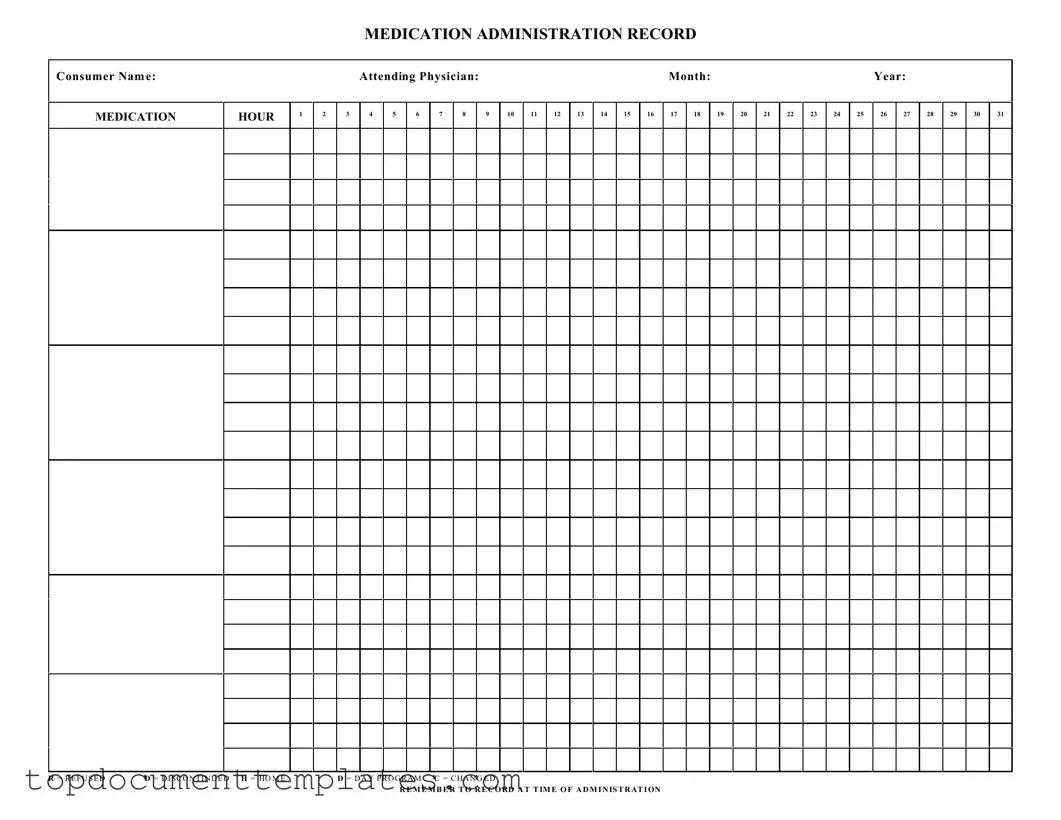
The Medication Administration Record Sheet is an essential tool used in healthcare settings to ensure that patients receive their prescribed medications accurately and on time. This form includes several key components, starting with the consumer's name and the attending physician's information, which helps identify the patient and their primary healthcare provider. It is organized by month and year, allowing for easy tracking of medication administration over time. Each day of the month is represented in a grid format, with designated spaces for recording the specific medications administered at various hours throughout the day. Additionally, the form includes notations for situations such as when a medication is refused, discontinued, or changed, which are marked with specific letters for clarity. This systematic approach not only aids in maintaining accurate records but also serves as a communication tool among healthcare staff, ensuring that everyone involved in the patient's care is informed about their medication regimen. Remembering to record the time of administration is crucial, as it contributes to a comprehensive understanding of the patient's treatment and adherence to their medication schedule.
Similar forms
The Medication Administration Record Sheet is a crucial tool for tracking medication administration in various healthcare settings. Several other documents serve similar purposes, ensuring accurate medication management and patient safety. Below is a list of documents that share similarities with the Medication Administration Record Sheet:
- Medication Reconciliation Form: This document is used to ensure that a patient's medication list is accurate and complete during transitions of care, similar to how the Medication Administration Record Sheet tracks administered medications.
- Patient Medication List: A comprehensive list of all medications a patient is taking, which helps healthcare providers verify and cross-reference with the Medication Administration Record Sheet.
- Prescription Order Form: This form contains details about medications prescribed to a patient. It is essential for understanding what should be included in the Medication Administration Record.
- Medication Error Reporting Form: Used to document any errors in medication administration, this form helps improve safety practices, much like the Medication Administration Record Sheet aims to prevent errors.
- Patient Care Plan: This document outlines the overall treatment goals for a patient, including medication management. It serves as a guide alongside the Medication Administration Record Sheet.
- Motor Vehicle Bill of Sale: A Motor Vehicle Bill of Sale serves as a crucial legal record for title transfers. It includes vital details that ensure clarity and protection for both parties involved, as detailed on documentonline.org/blank-motor-vehicle-bill-of-sale/.
- Administration Protocols: These guidelines provide detailed instructions on how to administer medications safely, complementing the information found in the Medication Administration Record Sheet.
- Medication Inventory Log: This log tracks the stock of medications available, ensuring that the medications listed on the Medication Administration Record Sheet are in supply.
- Incident Report Form: Similar to the Medication Error Reporting Form, this document captures any incidents related to medication, helping to enhance the safety measures reflected in the Medication Administration Record.
Guidelines on Writing Medication Administration Record Sheet
Filling out the Medication Administration Record Sheet is an important task that helps ensure proper medication management. Follow these steps carefully to complete the form accurately.
- Start by entering the Consumer Name at the top of the form.
- Next, fill in the Attending Physician's name.
- Indicate the Month and Year for the medication administration.
- In the MEDICATION section, list the names of the medications being administered.
- For each medication, note the hour of administration in the corresponding boxes.
- If a dose was refused, write R in the appropriate box. For discontinued doses, use D. If a dose was changed, mark C.
- Remember to record any notes at the time of administration to provide context for each entry.
Once you have completed the form, review it to ensure all information is accurate and clear. This will help maintain a reliable record for future reference.
Form Data
| Fact Name | Details |
|---|---|
| Purpose | The Medication Administration Record (MAR) is used to document the administration of medications to consumers in various healthcare settings. |
| Required Information | The form requires the consumer's name, attending physician, and a record of medication administration for each hour of the day. |
| State-Specific Laws | In many states, the use of MARs is governed by healthcare regulations, such as the Nurse Practice Act, which outlines the responsibilities of healthcare providers in medication administration. |
| Documentation Codes | Common codes used on the MAR include R for Refused, D for Discontinued, H for Home, and C for Changed, which help track medication status. |
Other PDF Documents
Can I Print Out a Ds-11 Form - There is no online submission option for the DS-11 form; it must be submitted in person.
Utilizing the Employee form not only streamlines the performance evaluation process but also ensures that the assessment is thorough and structured. This form can be indispensable for managers looking to provide feedback and identify areas for employee growth, thus enhancing overall team productivity. For more resources on employee management and forms, refer to OnlineLawDocs.com.
Us Service Animals Esa Letter - This document can be essential for accessing mental health resources and services effectively.
How to Make Pay Stubs If Self Employed - A useful document for business owners to maintain contractor compliance.